Alessandro Donà M.D. | Rocco Bonfatti M.D. | Chiara Manzini M.D. | Elisa De Santis Ph.D. | Gian Mario Micheloni M.D. | Andrea Giorgini M.D. | Giuseppe Porcellini M.D.
Introdution
Osteochondritis dissecans (OCD) is a rare acquired joint condition characterized by damage of the subchondral bone from a suspected ischemic cause with a secondary possible focal disruption with osteonecrotic evolution. It occurs primarily in young overhead athletes (e.g., those who participate in tennis, badminton, cricket, baseball, volleyball, weightlifting, gymnastics) between 6 and 20 years of age after a joint injury or a long period of sport activity, usually after repetitive overuse. (1)
Because of a lack of cartilage innervation and vascularization, symptoms are nonspecific and characterized by pain and crepitus and appear only when the innervated subchondral bone is damaged. Spontaneous healing is absent or very slow, with possible evolution toward a degenerative condition. Convex articular surfaces are generally involved, such as femoral condyles (especially the posterolateral part of the medial condyle), talar dome, and humeral head. Therefore, the most typically affected joints are the knee (75% of cases), the ankle, and the elbow: the shoulder represents approximately 1.6% cases of OCD. The humeral head is more involved than the glenoid, which conversely presents a concave, noneweightbearing articular surface. (2)
The etiology of OCD is poorly understood and plausibly multifactorial. Reduced blood flow attributable to vascular disruption from repetitive trauma is probably the main cause. Another important factor is represented by the particular relationship between the humerus and the glenoid in the overhead arm position: this implies an increased mechanical load from compressive forces across the glenohumeral joint accentuated by repetitive microtrauma.2 In particular, it has been hypothesized, at least in baseball players, that the humeral head is pushed posteriorly by the anterior band of the inferior glenohumeral ligament; this determines, over time, a compressive force on the glenoid that may lead to the onset of OCD. (2)
Moreover, a genetic component could be present, predisposing certain individuals to a greater possibility of developing the disease.
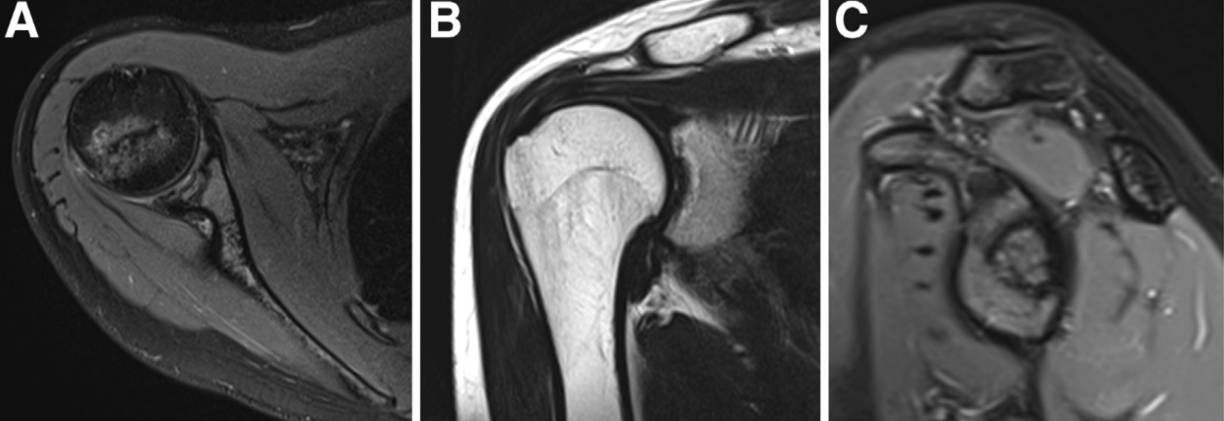
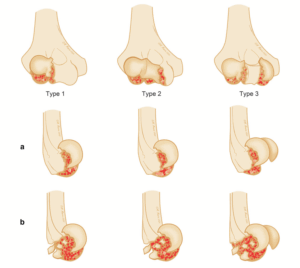
Recent studies have evaluated the progressive joint damage stages (from I to IV) according to the International Cartilage Research Society (ICRS) OCD grading on the basis of magnetic resonance imaging (MRI). (3)
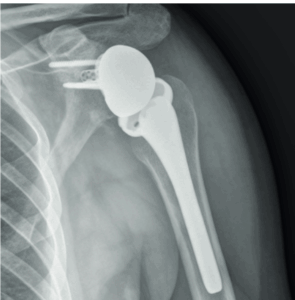
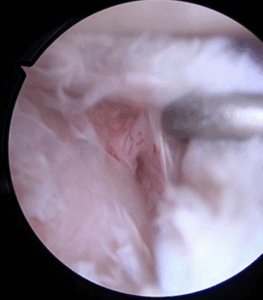
It was demonstrated that, despite the different concave shape of the glenoid, its OCD follows the same progression over the time of the convex weight-bearing articular surfaces and needs, likewise, the same gradespecific management. Patients with IRCS OCD stage I and some with OCD stage II present with a stable shoulder and can undergo conservative treatment. Unstable or advanced glenoid OCD stages, characterized by disruption of the articular cartilage and the presence of separated fragments as loose bodies, require surgical treatment. Moreover, this is indicated when the conservative approaches fail, especially because of long-standing pain and joint range of motion worsening. Proposed surgical treatments include arthroscopic drilling, microfractures, debridement of the unstable osteochondral fragments, and fixation with suture anchor or autogenous osteochondral plugs, platelet-rich plasma, and gellike sodium hyaluronate. (2,4) There is not yet consensus regarding the ideal technique. In this Technical Note, we describe an arthroscopic procedure with a single-layer hyaluronate-based scaffold for the treatment of OCD of the glenoid.
Clicca sul pulsante sottostante per continuare nella lettura dell’articolo completo e visualizzare le immagini di approfondimento.